the pressure-natriuresis (sodium excretion) curve
This article examines how salt intake affects blood pressure, emphasizing the kidneys’ role in regulating sodium excretion. In healthy individuals, blood pressure remains stable despite varying salt intake, but in hypertensive patients, higher blood pressure is required to excrete salt, leading to potential increases in blood pressure. The body uses mechanisms like renin suppression and hormone regulation to manage short-term blood pressure changes, but prolonged excessive salt intake can weaken these systems. The article also highlights the importance of accurate blood pressure measurements, particularly through home monitoring, for proper hypertension diagnosis and management.
The key factor in understanding the correlation between salt intake and blood pressure is the pressure-natriuresis (sodium excretion) curve. This curve illustrates the relationship between sodium excretion (= intake) and mean blood pressure.
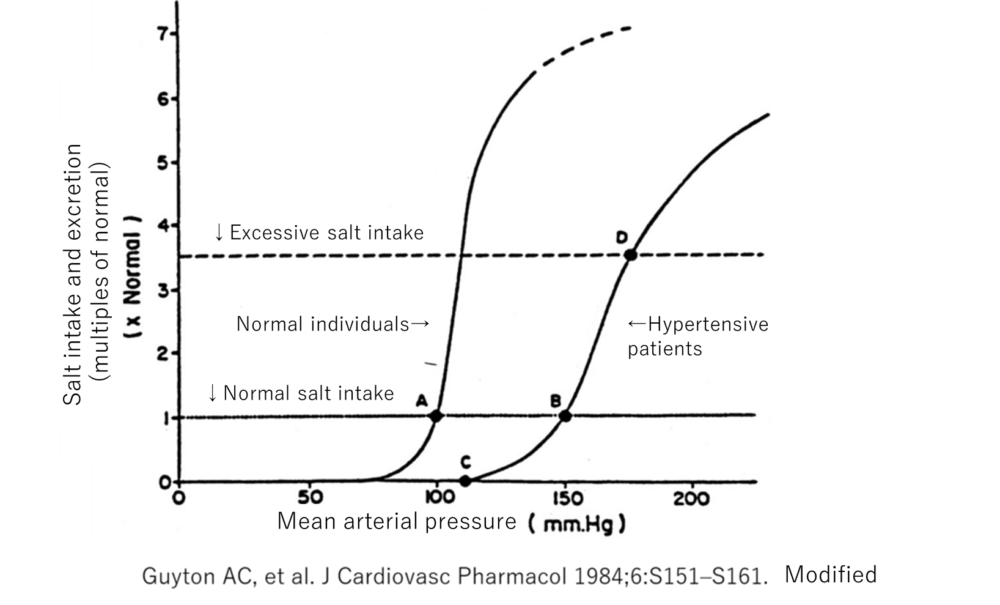
In the kidneys of a healthy individual, it has been shown that blood pressure remains nearly unchanged across a range of salt intakes, from normal to excessive. On the other hand, in hypertensive patients—those with a predisposition to salt-sensitive hypertension or those whose blood pressure easily rises due to factors such as slightly elevated pressor hormones or stiffening blood vessels—higher blood pressure is required to excrete the same amount of salt, even at normal intake levels. Furthermore, as salt intake increases, blood pressure rises almost proportionally. Individuals considered to be salt-insensitive exhibit less increase in blood pressure per unit of salt intake, but in hypertensive patients, blood pressure tends to rise to some extent with salt intake.
The critical point here is that the kidneys regulate mean blood pressure. Mean blood pressure is essential for maintaining electrolyte balance, which is necessary for salt excretion.
Salt Intake and the Body’s Response
First, salt is absorbed into the bloodstream (portal vein) through sodium channels, such as ENaC in the intestines. It then passes through the liver, reaches the heart, and is distributed throughout the body. After salt intake, the chloride concentration in the blood increases compared to pre-intake levels. This increase in chloride concentration is detected by the macula densa in the distal tubules of the kidney, leading to a decrease in renin secretion from the kidneys. Renin ultimately raises levels of angiotensin II and aldosterone, which increases blood pressure, promotes salt reabsorption in the kidneys, and triggers the body’s response to retain salt. Therefore, a decrease in renin results in the suppression of blood pressure elevation and salt reabsorption, thereby mitigating the rise in blood pressure caused by the transient increase in salt intake.
Angiotensin II controls the distribution of blood flow within the kidneys. The central part of the kidney is more developed in actively reabsorbing salt, while the outer part allows salt to pass through. Angiotensin II has the effect of directing blood flow to the kidney’s center to promote salt reabsorption. When angiotensin II is not acting, blood flow to the outer parts of the kidney is maintained, promoting salt excretion. Whether urine output increases is determined by the next factor, vasopressin.
Sympathetic Nervous System and Hormonal Changes
Salt intake, along with water absorption, increases venous return, which transiently increases cardiac output. When the arterial blood volume transiently increases, the vessel diameter expands, allowing the vessels to accommodate the increased blood volume. Some arteries (e.g., carotid and aortic arteries) have receptors that detect this change, leading to a reduction in sympathetic nerve activity, which in turn lowers blood pressure and reduces renin levels. Additionally, the heart has receptors that sense changes in the returning blood volume. When more blood returns to the heart, it stretches, triggering the release of hormones that promote the excretion of salt and water. These hormones also have a vasodilatory effect, reducing the blood returning to the heart.
By temporarily altering the levels of renin, sympathetic nerve activity, and heart hormones (such as ANP), the body adjusts to excrete salt appropriately. As salt levels rise, the osmotic pressure of the blood increases, which stimulates the release of the antidiuretic hormone vasopressin. Vasopressin acts on the kidneys to reduce urine output and causes blood vessels to constrict, raising blood pressure. It also stimulates the thirst center, prompting drinking behavior. Thus, while there are mechanisms to prevent an immediate rise in blood pressure following salt intake, persistent excessive salt intake can gradually diminish these mechanisms’ effectiveness.
In Hypertensive Patients
Essential hypertension refers to high blood pressure for which no clear cause has been identified under current medical knowledge. Among these cases, it is believed that sensitivity to salt plays a significant role. As medical science progresses, the mechanisms by which salt intake directly raises blood pressure may become clearer, allowing for more specific classifications of hypertension. Additionally, other sustained stimuli (such as smoking or psychological stress) that directly or indirectly affect blood pressure may also become more understood.
Diagnosing Hypertension
When hypertension is suspected, it is typically due to blood pressure measurements taken during health screenings or clinical visits. Blood pressure, like heart rate, varies throughout the day. It fluctuates even at rest and typically decreases during sleep at night. There is also a phenomenon known as “white coat hypertension,” where blood pressure increases when measured in the presence of medical staff.
Given these fluctuations, how should blood pressure be assessed to determine if one is hypertensive? The most accurate method, though not practical, would involve placing a pressure-measuring sensor directly in the artery and continuously monitoring it.
In heart failure patients, there is a system that monitors right ventricular pressure, which increases early in the process leading to symptoms like shortness of breath and edema. This involves placing a small sensor in the pulmonary artery, which transmits pressure data to an external device. If pressure exceeds a certain threshold, an alert is sent to the healthcare provider, prompting intervention.
For arterial pressure, such invasive monitoring is usually unnecessary because blood pressure can be accurately measured at locations like the upper arm, where external compression can occlude the artery. However, if safer sensors or external monitoring methods become available, 24-hour continuous measurement might be feasible, albeit limited to severe hypertensive patients.
Measuring Blood Pressure
There are three main methods for measuring blood pressure: (1) clinic blood pressure, (2) home blood pressure, and (3) 24-hour ambulatory blood pressure monitoring. Another method, though less reliable, is measuring blood pressure at external locations (e.g., gym or community centers).
Patients visiting an internal medicine clinic or undergoing a health checkup may have their blood pressure measured in a clinical setting, referred to as clinic blood pressure. The issue is that while guidelines for accurate measurement are established, it is challenging to adhere to these in everyday clinical practice or during health screenings. As a result, the obtained values may not always be reliable. Therefore, when accurate measurements cannot be ensured, it is crucial to also measure and evaluate home blood pressure.